Since the breakthrough led by Nikolai Anichkov a century ago, the feeding of cholesterol, and to an extent, dietary fat have been recognized as the sine qua nons for the dietary modification of experimental atherosclerosis, and have been used in thousands of experiments to successfully accelerate the development of atherosclerosis in mammalian, avian and fish species, not only of herbivorous, but also omnivorous and carnivorous nature.1 2 3 4 5 6 7 8 9 10 11 This includes the promotion of experimental atherosclerosis in over one dozen different species of nonhuman primates- New World monkeys, Old World monkeys, and great apes including the closest living relative to humans, the chimpanzee (Fig. 1).2 3 12 13 14 15 16 17 18 19 20 21 The atherosclerotic lesions induced by cholesterol feeding, including in the form of fresh eggs yolks in many opportunistic omnivores, such as various species of nonhuman primates, birds and pigs have been shown to closely resemble the disease in humans.1 2 3 4 22 23 24
 |
| Figure 1. Aortic atherosclerosis of a chimpanzee which died of a heart attack after long-term feeding of a diet rich in cholesterol and artery-clogging saturated fat |
It has also been observed that the long-term feeding of cholesterol and saturated fat has resulted in heart attacks, sudden death, development of gangrene, softening on the bones and numerous other serious complications in nonhuman primates.2 3 25 26 27 28 For example, it has been shown that when diets rich in cholesterol and saturated fat are fed to monkeys of the genus Macaca, including the rhesus monkey and the crab-eating macaque, they experience heart attacks at approximately the same rate as high-risk populations living in developed nations.3
In species that are unlike humans, very resistant to dietary induced elevations in LDL cholesterol, such as the order of the carnivora, unless LDL-receptor deficient breeds are used atherosclerosis is typically induced by raising serum (blood) cholesterol with a diet with very large amounts of dietary cholesterol, and either containing thiouracil or deficient in essential fatty acids.9 10 29 As noted by Steinberg:30
The point is very clearly made: the arteries of virtually every animal species are susceptible to this disease if only the blood cholesterol level can be raised enough and maintained high enough a long enough period of time.
Long-term feeding of cholesterol in relatively small amounts has actually been shown to induce atherosclerosis in rabbits, chickens, pigeons and monkeys despite only small or insignificant increases in serum cholesterol.1 4 13 Armstrong and colleagues conducted an experiment ‘designed to demonstrate a null point of the effect of dietary cholesterol on the arterial intima’, by comparing a group of rhesus monkeys fed a cholesterol-free diet with a group fed cholesterol equivalent to that found in only half of a small egg in the average human diet of 2,000 calories per day (43µg/kcal). However, even when fed in very small amounts dietary cholesterol still had a significant adverse effect on these monkeys arteries after a period of only 18 months (Fig. 2).13 Armstrong and colleagues concluded:
No null point for the effect of dietary cholesterol on arterial intima was found even at an intake level far below that conventionally used for the induction of experimental atherosclerosis in the nonhuman primate. The intimal changes found in response to very low cholesterol intake imply that subtle qualitative alterations in lipoproteins are of critical importance to our understanding of lesion induction.
 |
| Figure 2. Subclavian artery from a rhesus monkey fed very small amounts of dietary cholesterol (43µg/kcal). Sudanophilia (black area) is intense in the area of major intimal thickening |
It has also been demonstrated that the cessation of a cholesterol-rich diet and the subsequent lowering of serum cholesterol results in the regression of atherosclerosis in various mammalian and avian species, including herbivores, omnivores, carnivores and nonhuman primates.31 In one experiment Armstrong and colleagues induced severe atherosclerosis in rhesus monkeys by feeding a diet with 40% of calories from egg yolks for 17 months. The egg yolks were then removed from the monkeys diet and replaced with a cholesterol-free diet with either 40% of calories from corn oil or low-fat chow with 77% calories from sugar for three years, resulting in a reduction of serum cholesterol to <140 mg/dl and a marked regression of atherosclerosis.32 33
In a recently published study, Spence and colleagues observed that egg yolk consumption was associated with carotid plaque in high-risk patients.34 These findings should not come as a surprise considering the evidence accumulated from thousands of animal experiments over the last 100 years, which have demonstrated that the feeding of cholesterol and saturated fat accelerates the development of atherosclerosis in virtually every vertebrate that has been sufficiently challenged. These lines of evidence have been neglected by the egg industry and promoters of cholesterol laden diets (ie. Paleo, Primal and low-carb) who have attempted to discredit this study without considering the relevant evidence. As noted by Stamler:35
To neglect this fact in a review about humans is to imply that the Darwinian foundation of biomedical research is invalid and/or that there is a body of substantial contrary evidence in humans. Neither is the case.
These findings from Spence and colleagues are not only supported by the findings from animal experiments, but also by numerous previous human studies that found a positive association between dietary cholesterol and the severity of atherosclerosis.36 37 38 39
In the video below Dr. Michael Greger addresses the completely unethical measures that the egg industry resorted to in order to confuse the general public about these findings from Spence and colleagues, including attempts to bribe researchers.
Eggs vs. Cigarettes in Atherosclerosis
In the video below Plant Positive addresses various critiques of Spence and colleagues findings, as well as other relevant research on dietary cholesterol.
Cholesterol Confusion 6 Dietary Cholesterol (And the Magic Egg)
Eggs, Cholesterol and Xanthomatosis
In addition to developing atherosclerosis and gangrene, the feeding of egg yolks and cholesterol to various species of nonhuman primates has also resulted in the development of xanthomatosis, a condition where deposits of cholesterol develop underneath the skin and is associated with chronically elevated serum cholesterol.18 40 41 42 43 This condition has been shown to be cured in nonhuman primates upon the cessation of a cholesterol-rich diet.41 A case report found that a 30-year-old woman with a healthy body weight who had been following a carbohydrate restricted diet for three and a half years had developed xanthomas on her hands and a chronically elevated serum cholesterol level of 940 mg/dl.44 The composition of the woman’s diet was reported as follows:
Each day she had consumed eight to 12 eggs, one or two lean steaks or half a small chicken and, half to one litre of milk. Sometimes some cottage cheese or tomatoes enriched the menu and, on rare occasions, fruit. She completely avoided butter, bread, potatoes, rice, noodles, alcohol, or any other food or beverage containing carbohydrate. The daily cholesterol intake, which was mainly derived from the egg yolks, was about 3500 mg. The total calorie intake was about 8-4 MJ (2000 kcal) (35 % protein, 55 % fat, and 10 % carbohydrates, polyunsaturated fat:saturated fat (P:S) ratio=0 26).
The woman was advised to change her diet, and in particular to stop eating eggs. After 16 days her serum cholesterol dropped to 750 mg/dl, and after several years dropped to 188 mg/dl and the lipid deposits on her skin had cleared up. This woman’s diet induced xanthomas and chronically elevated cholesterol resemble the characteristics of people with homozygous familial hypercholesteromia, a rare genetic disorder that results in chronically elevated concentrations of predominantly large LDL cholesterol particles.45 People with this disorder are short lived and often experience heart attacks during childhood.46 Such unfavorable risk factors would normally be of great concern to any responsible physician. However, despite the overwhelming evidence of the danger of elevated serum total and LDL cholesterol,30 47 48 including for women,49 50 Sally Fallon and Mary Enig, the founders of the Weston A. Price Foundation claim that ‘For women, there is no greater risk for heart disease, even at levels as high as 1000 mg/d’.51 It is clear that this organization has little concern for the wellbeing of people.
Eggs, Cholesterol and Serum Lipids
It has been well established in rigorously controlled feeding experiments that adding dietary cholesterol to a diet that is low in cholesterol can significantly raise serum cholesterol in humans.52 An addition of 200 mg cholesterol per day to a cholesterol-free diet has been shown to raise serum cholesterol by as much as 20%.53 This may be largely explained by the strong evidence that dietary cholesterol down-regulates the LDL receptor.54 However, as Hopkins addressed in a meta-analysis of rigorously controlled feeding experiments, there exists a ceiling effect at which adding additional dietary cholesterol to a diet already rich in cholesterol has little appreciable effect on serum cholesterol (Fig. 3). Therefore, the fact that numerous studies carried out on populations with a relatively high baseline cholesterol intake failed to find a significant association between cholesterol intake and serum cholesterol does not negate the evidence that lowering intake to near zero will significantly lower serum cholesterol.
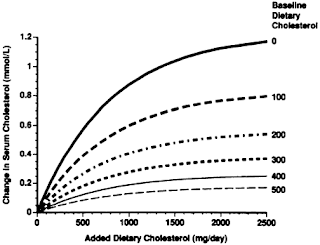 |
| Figure 3. Effects of added dietary cholesterol on serum total cholesterol at different baseline levels of intake |
Several controlled experiments have found that overweight compared to lean people, and insulin resistant compared to insulin sensitive people are less responsive to dietary cholesterol.55 56 This likely explains why researchers who have financial or personal connections with the egg industry have specifically selected overweight and insulin resistant participants with a modestly high baseline dietary cholesterol intake for controlled trials, as it can be pre-empted that this subgroup of the population will show little response when egg intake is increased.
It has been demonstrated in multiple meta-analyses of rigorously controlled feeding experiments that dietary cholesterol, including that from eggs yolks does have a modest adverse effect on the LDL:HDL cholesterol ratio.57 58 Furthermore, unlike for LDL cholesterol, there is limited causal evidence that simply raising HDL will lower the risk of coronary heart disease. For example, a meta-analysis of 108 randomized controlled trials found that while lowering LDL cholesterol significantly decreased the risk of coronary heart disease and all-cause mortality, modifying HDL had little appreciable effect after controlling for LDL cholesterol.47 In addition, a recent meta-analysis of mendelian randomization studies found that while genetically modified LDL significantly influenced the risk of coronary heart disease, genetically modified HDL had little appreciable influence.59 This evidence together with the evidence that dietary cholesterol adversely influences both concentrations of LDL as well as the LDL:HDL ratio, especially in healthy people reinforces the recommendations to limit egg and cholesterol intake.
Another contributor to confusion caused by studies typically influenced by the egg industry is the suggestion that dietary cholesterol does not increase the number of LDL particles, or only increases the concentration of large LDL particles, which is considered by some to be less atherogenic. However, as elaborated by Plant Positive, several studies not influenced by the egg industry have found that cholesterol intake does increase the total number of LDL particles in healthy people.60 61 In addition, a systematic review found that higher LDL particle number, but not other LDL subfractions was consistently associated with an increased risk for cardiovascular disease, independent of other lipid measurements.62 The National Lipid Association Expert Panel recently concluded that ‘All lipoprotein particles in the LDL fraction are atherogenic, independent of size’, and was unable to identify any patient subgroups in which LDL subfraction measurements are recommended. In specific, the panel provided the following evidence for these conclusions:63
Studies have linked large LDL particles to atherosclerosis in nonhuman primates, in patients with familial hypercholesterolemia (who have an elevated concentration of predominantly large LDL particles), in participants of the population-based MESA study, in normolipidemic men with CHD, and among patients after MI [heart attack] in the Cholesterol And Recurrent Events (CARE) study... Many studies document links between small dense LDL particles and atherosclerotic CVD. However, these statistical associations between small, dense LDL and CV [cardiovascular] outcomes are either significantly attenuated or abolished when the analyses are adjusted for the overall number of circulating LDL particles (LDL-P) either by adjustment for Apo B levels or by adjustment for nuclear magnetic resonance-derived LDL-P... To date, there is no evidence that the shift in LDL subfractions directly translates into change in disease progression or improved outcome.
More recently a meta-analysis of mendelian randomization studies with over 312,000 individuals found that inheriting any of nine studied genetic variants that modify lifelong LDL cholesterol concentrations, but not any other known risk factors predicted a 55% lower risk of coronary heart disease for each mmol/l (38.7 mg/dl) lower LDL cholesterol.48 Despite having significantly different effects on LDL particle sizes, all of the nine studied genetic variants predicted essentially the same decrease in coronary heart disease per unit lower LDL cholesterol, including the gene responsible for familial hypercholesterolemia which elevates predominantly large LDL particles.45 Therefore there is convincing evidence that large LDL particles promote atherosclerosis.
The elevation of LDL cholesterol is not the only adverse effect that increased intake of eggs and cholesterol confers. As Spence and colleagues also pointed out in regards to recent controversy surrounding dietary cholesterol:40 64
The elevation of LDL cholesterol is not the only adverse effect that increased intake of eggs and cholesterol confers. As Spence and colleagues also pointed out in regards to recent controversy surrounding dietary cholesterol:40 64
Focusing on fasting serum cholesterol levels misses the bulk of the problem. Even though serum cholesterol rises very little after a meal, dietary cholesterol increases the susceptibility of LDL-C to oxidation, vascular inflammation, oxidative stress, and postprandial hyperlipemia and potentiates the harmful effects of saturated fat, impairs endothelial function, and increases cardiovascular events.
Classical Observations
Multiple international studies based on data from the World Health Organization have found the mean per capita dietary cholesterol levels are consistently associated with the rates of coronary heart disease mortality.39 65 This includes a large study of 40 countries.66 Similarly, it was found in the 25 year follow-up of the Seven Countries Study that dietary cholesterol was associated with a significantly increased risk of coronary heart disease across the 16 cohorts.67
In a review of the literature, Uffe Ravnskov, the spokesperson for The International Network of Cholesterol Skeptics reviewed 15 of the earliest prospective (longitudinal) cohort studies and inappropriately concluded that ‘Overall, longitudinal studies within population have found no difference between the diet of coronary patients and others’.68 Fourteen of these studies measured cholesterol intake, of which for the Chicago Western Electric Study Ravnskov inappropriately cited data from an earlier follow-up that found no association rather than the longer follow-up which found a significant association. Among the remaining thirteen studies, the participants who developed coronary heart disease actually had on average 13 mg/day greater intake of cholesterol for someone consuming on average 2,000 calories a day.
Considering the probable degree of measurement error dietary intake and the fact that these studies were carried out in largely homogenous populations where most people had similar diets, only relatively small differences in dietary composition would have been expected between participants with and without heart disease even if diet does play a major role in heart disease [reviewed previously]. Furthermore, Ravnskov failed to mention that four of the largest studies that he cited, including the Chicago Western Electric Study found on average that 200 mg/1,000 calories higher intake of cholesterol was associated with a 30% increased risk of coronary heart disease over and above the adverse effects it has on serum cholesterol.64
The next post in this series will focus on findings from more recent prospective cohort studies that addressed the intake eggs and cholesterol and the risk of coronary heart disease, diabetes, heart failure, cardiovascular disease and all-cause mortality. Many of these important findings have gone unaddressed in recent reviews of the literature.
Diet-Heart Posts
Part I - Diet-Heart: A Problematic Revisit






0 komentar